Servo Ventilator story
The pioneer of personalized mechanical ventilation
Many of the innovations in mechanical ventilation that we take for granted today are the result of the Servo Ventilator history. Groundbreaking technology and partnerships with visionary clinicians are some of the things that have made this possible.
Servo Ventilator - The pioneer of personalized mechanical ventilation
A world’s first – a small electronic ventilator that was flow-controlled, and enabled clinicians to reliably achieve set tidal volumes through its rapid Servo Control System.
Read moreIntroduced enhanced monitoring of respiration and gas exchange, synchronized ventilation and facilities for managing ventilation of children and newborn babies.
Read moreThe first ventilator on the market which precisely could control airway pressures throughout inspiration and expiration by introducing Pressure Control and Pressure Support.
Read moreThe first universal ventilator enabling treatment of all patient categories, from adults to premature neonates. Gave birth to the Volume-target ventilation modes PRVC and VS.
Read moreServo-i: The first ventilator system designed as an upgradeable mobile and modular platform. Servo-s: A straightforward and cost-effective package utilizing cutting edge technology.
Read moreServo-u: First ventilator with all-touch user interface to provide higher levels of patient safety and a superior user experience[14]. Servo-n: Purposely created as an all-in-one neonatal ventilator
Read moreThe first turbine-driven Servo Ventilator with a gentle and sensitive non-invasive ventilation (NIV), ideally suited for intensive and intermediary care as well as intra-hospital transport.
Read more
100 years of Swedish respirator development
At the University Hospital of Lund in the of Sweden, groundbreaking innovations such as echocardiography (Edler/Hertz) and the single-use artificial kidney (Alwall) had seen the light of day. In Lund, there was also a tradition of inventing respirators, such as the Barospirator (an iron lung variant,1920), the Sahlin-Stille cuirass-respirator (1930) and the Lundia-respirator (1953). The rich Swedish respirator history also had seen development of respirators in Stockholm, the Spiropulsator (1936), which was the first electric respirator integrated in an anesthesia apparatus, and the Engstrom respirator, used for the first time in Copenhagen, Denmark, during the major polio outbreak in 1952, instigating the paradigm shift from negative- to positive-pressure ventilation, and being the first volume-controlled respirator.
Forming of the Servo Ventilator team
In 1965, Professor Sven Ingelstedt at the Department of Clinical physiology granted a request from the young doctor Björn Jonson to develop a new respirator under an ambiguous directive that Sven had formulated “Respirators are pressure- or volume controlled. They should be flow controlled. Then we could do what we want! P.S. It is not possible to control flow!” The core project team was later completed with anesthesiologist Dr. Lars Nordström and the ambitious electrical engineer Sven-Gunnar Olsson employed by Elema-Schönander, a company outside Stockholm famous for having invented the electrocardiogram inkjet printer (1948) and the implantable pacemaker (1958). The project was given wide degrees of freedom and experimentation in an environment that fostered cross-institutional teamwork and entrepreneurship.

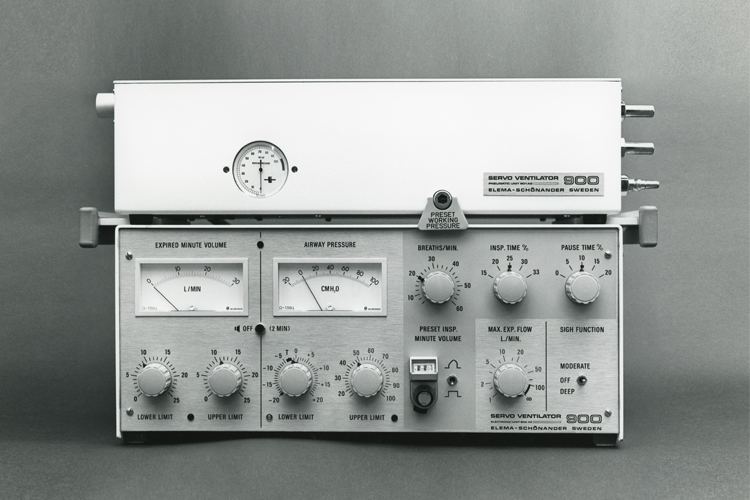
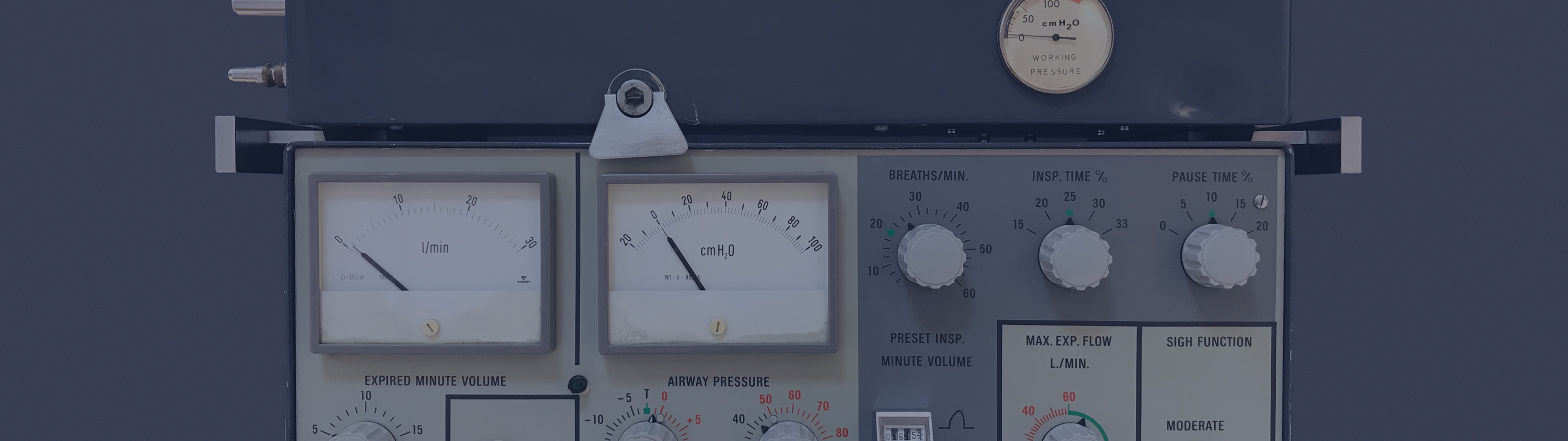
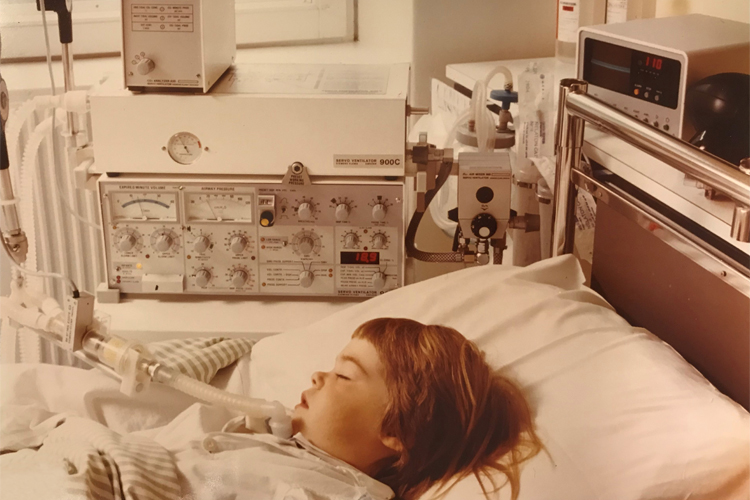
1971 - Servo Ventilator 900
The Servo Ventilator 900 became a world’s first – a ventilator that was flow-controlled and could provide respiratory monitoring of vital parameters and gas delivery. A small, silent, electronic device that would enable the clinician to reliably achieve set tidal volumes by delivering accurate flow to the patient through its rapid Servo Control System, independent of changes in resistance and compliance of the patient´s respiratory system. The term Ventilator was introduced to emphasize that it involved new principles which gave clinicians the possibility to provide the best ventilation method for each patient including infants.
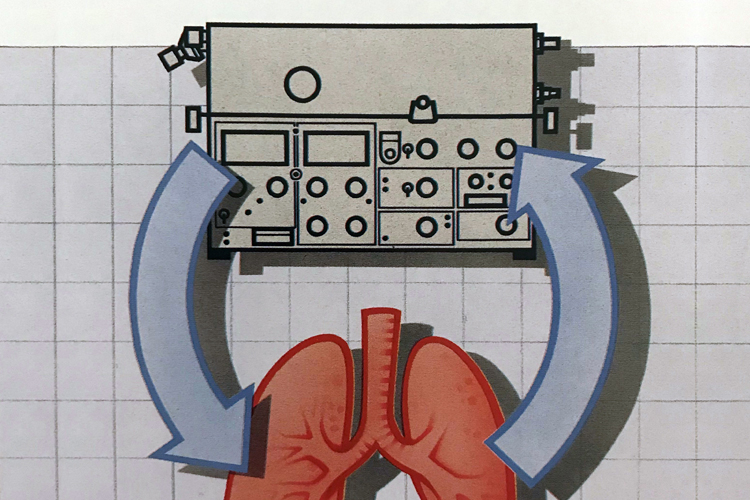
1971 - Servo Control System
The brain of the Servo Ventilator was the unique Servo control system, which through application of state-of-the-art electronics contributed to a great flexibility in operation and the choice of properties for the ventilation modes. Pressure and flow sensors in the patient gas delivery circuit with a very small compressible volume, fed information back to the inspiratory and expiratory valve units several hundred times per second. Visual and audible alarms were immediately activated if pre-set limits for airway pressure and expiratory minute volume were exceeded.

1973 - Lung mechanics calculation
A real clinical breakthrough was the integrated monitoring capabilities of the Servo Ventilator, where the Lung Mechanics Calculator 940 provided six different parameters and served as an aid in choosing the best setting of the ventilator on a breath-by-breath basis. A key area of interest was how to set the external PEEP-valve to achieve the best effect on end-expiratory lung volume and oxygenation. The Servo Ventilator also made recording and data export possible, which made it the preferred ventilator choice for research in mechanical ventilation, testified by the increasing amount of scientific publications during the 70s.
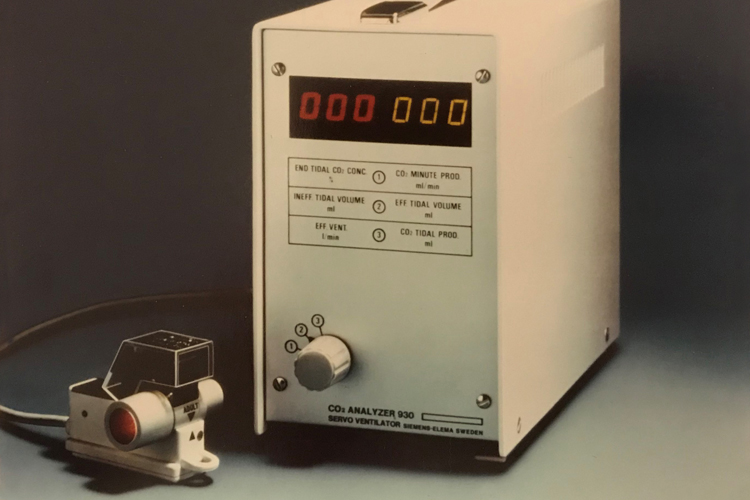
1974 - Carbon dioxide analysis
In the ICU there was a need to continuously measure CO2 as a surrogate for the arterial blood gas pressure PaCO2, which was considered to be time-consuming and expensive. The CO2 Analyzer 930 was the first commercial volumetric capnograph and was based on measurement of IR light absorption in a small and fast mainstream sensor connected to the ventilator. This provided real-time breath-by-breath end-tidal CO2 concentration, CO2 tidal minute elimination, and deadspace calculations. It provided an invaluable contribution in guiding ventilator settings and to the understanding of severity of pulmonary disease, gas distribution in the lungs, circulation and metabolism.

1976 - Servo Ventilator 900B
The successor to the Servo 900 came to be known as the Servo 900B. It introduced an Intermittent Mandatory Ventilation (IMV) mode which was synchronized to the patient´s respiratory efforts, who was in-turn encouraged to take over more and more of the respiratory workload. Subsequently the weaning process became less painful, both physically and mentally. Additionally CPAP capability, extended setting ranges and the default “green settings” were implemented on the front panel. Hospitals around the world began to recognize that the Servo Ventilator was not purely designed for adults, but unlike contemporary ICU ventilators, also offered the facilities for managing children and newborn babies.
1981 - Servo Ventilator 900C
The Servo 900C, introduced in 1981 as the “Limitless Servo Ventilator System”, and like its predecessors it had been designed to be easy to learn, set, place, clean and service. It was the first ventilator on the market which truly could control airway pressure precisely throughout inspiration and expiration. Electronical control of PEEP, and eight different ventilation modes, which also could be run in an accentuated infant patient range were now available. CPAP could now be delivered through the ventilator with supervision of minute ventilation and CO2 exchange. Extensive training material (“The Servo University”) with application booklets, demonstration panel, deck of patient cards, videos and a clear and consistent operating manual were integral parts of the limitless program.
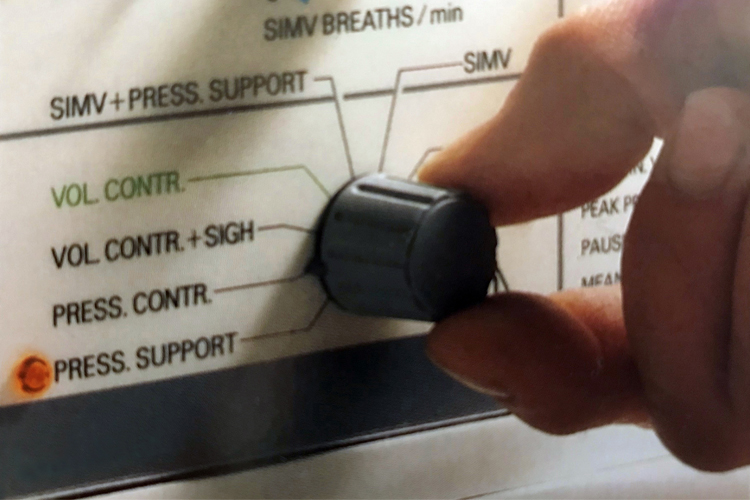
1981 - Pressure Control (PC)
Originally named Servo Pressure Control Ventilation, its delivery of constant inspiratory pressure with a decelerating flow pattern was able to prolong the time for gas exchange in the alveoli while it was expected to reduce the risk of barotrauma compared to traditional volume controlled ventilation. Very high peak pressure was common before the current era of low-tidal volume ventilation. The Pressure Control also quickly became popular for uncuffed pediatric and neonatal patients).
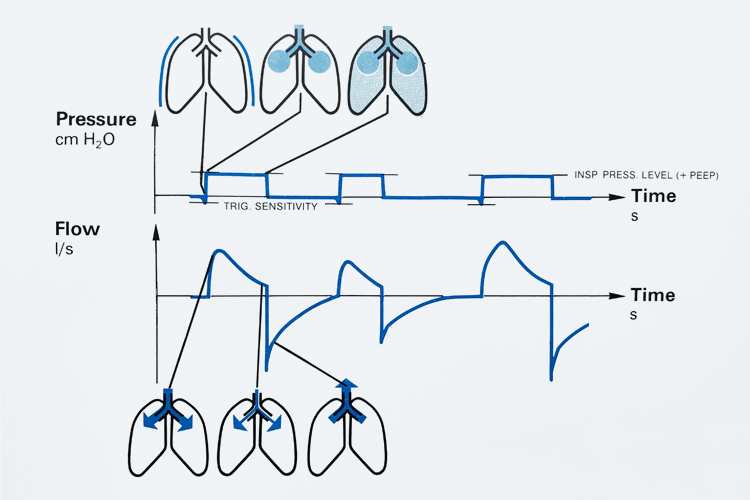
1981 - Pressure Support (PS)
Introduced to the intensive care world in the Servo 900C, and in less than 10 years after its inception, Pressure Support Ventilation became the new standard mode for weaning. It was an important step in allowing the patient to take increased control of the timing of the ventilatory support, while the ventilator took over most of the respiratory work. The engineers worked with several criteria to solve the timing problem, and finally decided that the flow decay during a pressurized breath was probably the best variable to use. Breath termination at 25% of the peak flow was determined to be the most comfortable level of support, as indicated by their own experience. Research on the potential clinical benefits of Pressure Support immediately took off and was a major topic in scientific articles for many years to come.
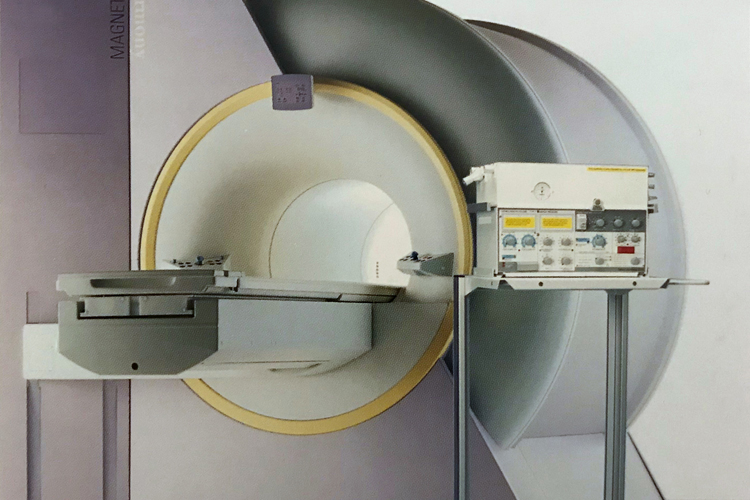
MRI Conditional use
Magnetic Resonance Imaging (MRI) was a novel and revolutionary imaging technique emerging in the early 1980’s. The environment required by the technology was a challenge for the construction of the MR-suite and also for equipment that was brought in as magnetic items could pose a serious risk. Many patients with potential benefit of an MRI examination required mechanical ventilation. The Servo 900C had few magnetic parts, and was the first ventilator that was released for use in this environment. It has later been followed by MR-versions of the latest Servo Ventilator generations.
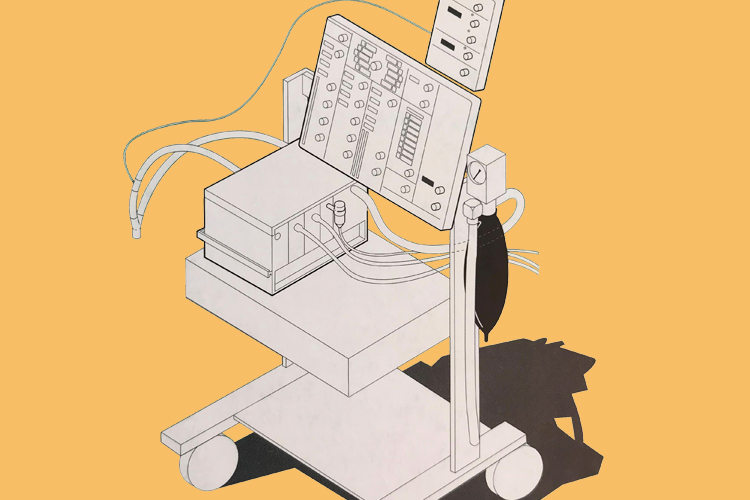
1991 - Servo Ventilator 300
The Servo 300 series represented a giant technological advancement and constituted a leap into the microprocessor era, as the first universal ventilator enabling treatment of all patient categories, from adults to tiny premature neonates. It included a completely new and unique gas delivery system with gas modules for air and oxygen and a small mixing chamber. The new sensitive flow-triggering system with rapid flow response gained a lot of interest due to its capability to reduce work-of-breathing. Servo 300 also set a new benchmark for tidal volume delivery by going down to 2 ml.
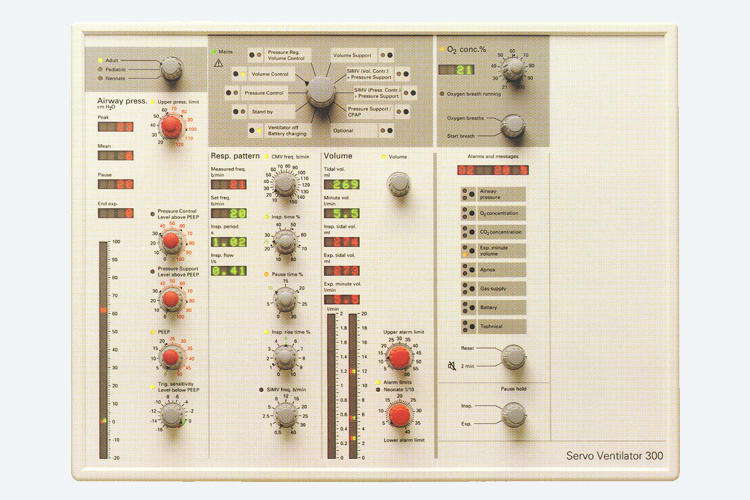
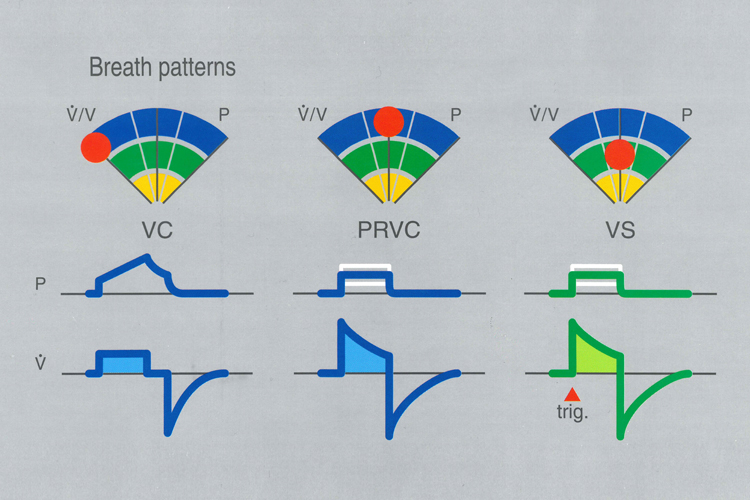
1991 - Volume-targeted Ventilation (PRVC and VS)
Through each cycle of Servo Ventilator generations there has been an inherit drive to invent ventilation modes that would meet increasing clinical needs of the future. The Servo 300 launched a set of Volume-target modes; Pressure Regulated Volume Control (PRVC) and Volume Support (VS), where the key principle was to deliver the set volume at the lowest required inspiratory pressure, targeted on a breath-by-breath basis. Neonatal and pediatric ICUs quickly embraced Volume-targeted Ventilation as it became clear that this particular innovation would offer the transition from less precise and unpredictable pressure-limited continuous flow ventilation modes.
1991 - Servo Ventilator 300 NO
The Servo 300 also came in a unique version which addressed the growing interest in nitric oxide (NO) therapy, as a potent vasodilator to improve oxygenation in very severe patient groups, including prematures with pulmonary hypertension. NO delivery and monitoring were fully integrated and a third gas module provided precise NO dosing in full synchrony with the breath delivery. Due to an exclusive patent licensed to a Swedish gas manufacturer for the medical use of NO for treatment of lung dysfunction, production of until then unmatched Servo 300 NO delivery system was forced to be discontinued.
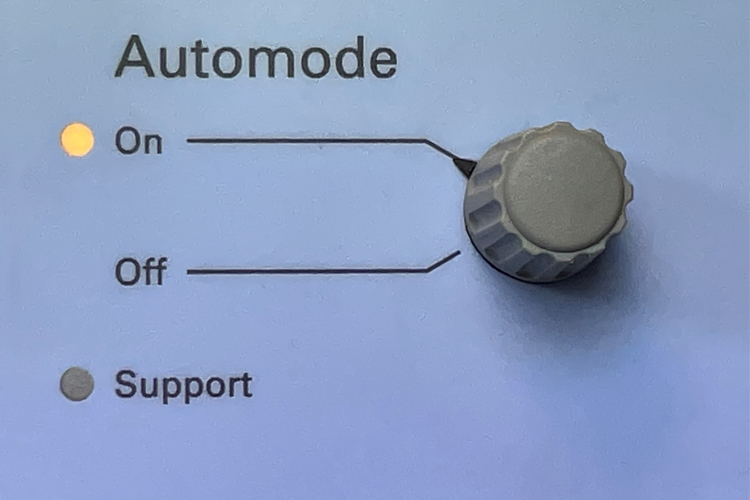
1996 - Automode®
In the pioneering search for more gentle and patient-friendly ventilation, the next step was the Automode function, developed to form a bridge between controlled and spontaneous ventilation in the early weaning process. Automode incorporated three combinations of control and support modes, and was automatically switched back and forth seamlessly supervised by an adaptive apnea time algorithm. The benefits were clear: reduced sedation requirements, less operator intervention and less alarms. Weaning could be started earlier and patient activity was always rewarded without requiring intervention from the staff. The front of the Automode brochure progressively stated “Weaning begins with intubation.
1998 - Open Lung Tool®
Research with the aim to reduce ARDS incidence and mortality heralded the implementation of the Open Lung Tool which by using breath-by-breath trends of parameters such as Dynamic compliance and CO2 elimination provided quantification of the effect of interventions, in particular alveolar recruitment maneuvers. Through a stepwise approach including a decremental PEEP titration, the PEEP setting could now be personalized to achieve improved oxygenation with ventilation at the lowest possible driving pressure, with a homogenous lung volume. The Open Lung Tool would also indicate when lungs were not recruitable, and other approaches should be considered and evaluated.

1999 - Neurally controlled ventilation
In December 1999, a new dimension of ventilation technology was presented in Nature Medicine, where a group lead by Dr. Christer Sinderby at the University of Montreal described how progress in signal acquisition and processing of the electrical activity of the diaphragm (Edi), meant that it could be used to allow the patient´s own respiratory center to assume full control of the timing and magnitude of the respiratory support provided by the ventilator. Establishment of full patient-ventilator synchrony and use of intrinsic lung-protective reflexes, provided new hope for adult and pediatric intensive care ventilation for the 21st century. The vision outlined reduction of ventilator-related complications, facilitation of weaning in order to decrease ICU and hospital length of stay. Visionary Servo people saw the potential of the technology, which was initially deployed on a Servo 300-based prototype.
2001 - Servo-i Ventilator System
A a result of unprecedented cooperation with clinicians worldwide, Servo-i became first ventilator designed as a mobile and modular platform, intended to frequently bring new clinical functionality and upgrades to the already installed ventilator fleets. The innovative system approach included three main configurations - Infant, Adult and Universal. New levels of flexibility in placement, handling and support, during intrahospital transport was offered through a comprehensive range of smart accessories, and uninterrupted connectivity. The user interface now allowed the users to choose between touch screen, a main rotary dial and direct access knobs provided secure control of the most vital settings. This was combined with up to five color-coded high-resolution waveforms with diagnostic quality.

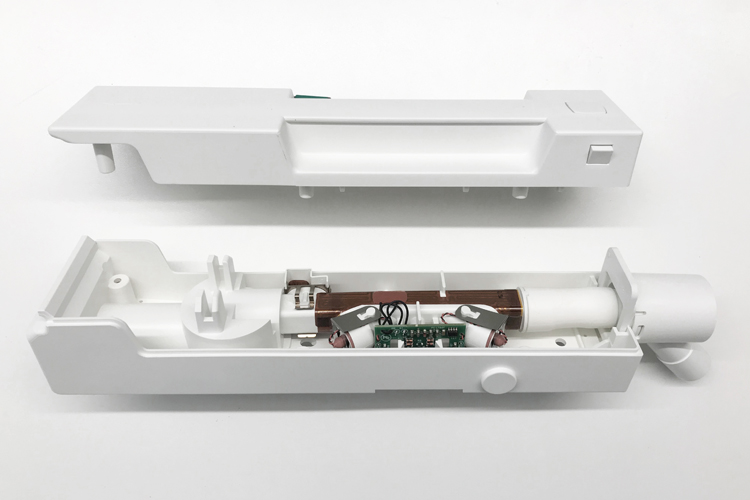
Ultrasonic Expiratory Flow Sensor
The new one-piece Expiratory Cassette would meet increasing customer demands regarding reliability and re-processing, and introduced a brand new technology seen for the first time in Servo ventilators, namely Time-of-flight Ultrasound. Its ultra-fast measurement was virtually independent of gas composition and humidity. The huge success of the ultrasonic flowmeter also lead to the development of an Ultrasonic Oxygen Sensor, which could work over the lifetime of the ventilator. The technology was also later found to be effective for detection of the low density Heliox gas mixture, when it later was implemented as the third supply gas for the Servo-i.
2003 - Servo-s Ventilator System
Servo-s brought cutting edge technology from its big brother Servo-i, into a straightforward and cost-effective package, presented under the tagline “Simplicity makes sense”. It was appropriate for a variety of hospital ventilatory care settings, and in combination with quiet and compact Compressor Mini it was able to deliver high-quality ventilation independent of central wall gas. The user-friendly simplicity, state-of-the-art performance and reliability for both adult and pediatric patients, made the Servo-s an instant success in the emerging BRIC economies (Brazil, Russia, India and China), looking for high-value medical devices when modernizing their healthcare systems.

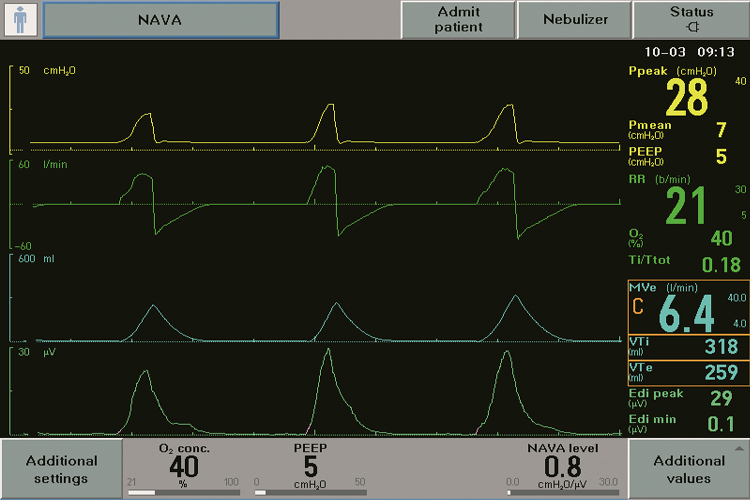
2007 - NAVA (Neurally Adjusted Ventilatory Assist)
The introduction of NAVA in Servo-i, featured plug-in HW and SW modules, as well the Edi catheter also functioning as nasogastric feeding tube, was nothing short of a sensation! Coinciding with the introduction of scientific papers showing the deleterious effects of patient-ventilator asynchrony, associated problems due to increased sedation and the findings that VIDD (Ventilator-induced Daphragm dysfunction) was a real problem in ventilated patients. Since then, NAVA has been shown to address these problems by shortening the time of mechanical ventilation[1] and increasing the number of ventilator-free days [1] [2] [3] by providing personalized ventilation that is both lung- and diaphragm-protective.
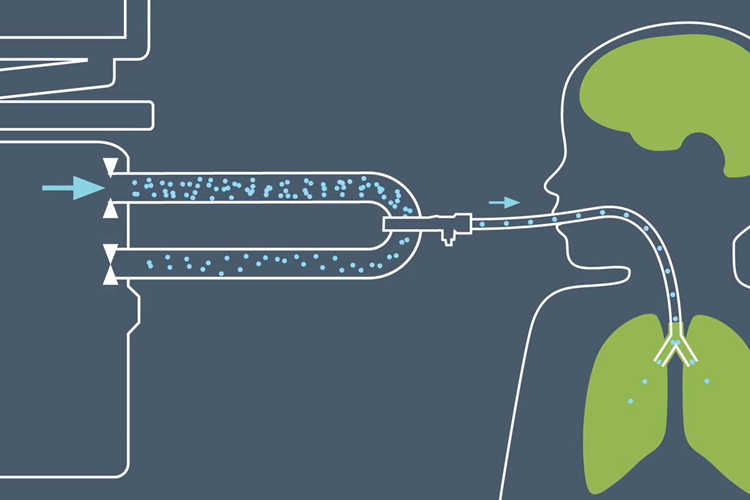
2010 - NIV NAVA
As NAVA compared to traditional ventilation modes, is independent of leaks, the application of non-invasive ventilation (NIV NAVA) was the natural step to take as paradigm shift in treatment to patient groups traditionally treated with more invasive modes. NIV NAVA's continuously growing application in neonates has been tremendous, where its success is based on that it may prevent intubation [4][5], or allow early extubation [6][7][8] when compared to conventional NIV modes which are not sufficiently synchronized. Another patient group benefitting are adult patients with acute exacerbation of COPD, in which NIV NAVA has been shown to reduce NIV complications, and may be effective in managing the patients status and also to improve outcomes. [9][10][11][12][13]


2014 - Servo-u Ventilator System
Every new generation of Servo Ventilator has been expected to transform how ventilators are perceived within industry. Servo-u successfully introduced a highly intuitive all-touch user interface with context-based guidance and workflows, recommendations and shortcuts. The objective was to make implementation of advanced ventilation strategies easier to implement in daily practice through enhanced user confidence. New important monitoring parameters, such as VT/PBW and Driving Pressure were implemented, both continuously visualized in the Servo Compass. New options for personalized lung protection and weaning for treatment of all patient categories, from neonates to adults were added. A comparative study of ventilator usability showed higher levels of patient safety and a superior user experience [14].
2014 - Servo-n Ventilator System
Servo-n was purposely created as an all-in-one neonatal ventilator to help provide vulnerable neonates with the support they needed while protecting the lungs, respiratory muscles and other developing organs [15]. Dedicated exclusively to neonatal ICU’s and to build confidence for both parents and caregivers, it includes aesthetic details like the green ladybug and the unique Family view. Compensation for variable leakage in all invasive modes, an optional hot-wire flow sensor as well as the integrated possibility to run High Flow oxygen therapy had been added. Both NAVA and NIV NAVA are of course standard modes, where the continuous Edi signal plays an essential role in monitoring and managing apnea of prematurity in order to prevent desaturation and bradycardia [15][16][17].


2015 - Servo-air Ventilator System
The Servo-air became the first turbine-driven Servo Ventilator with powerful “hot-swappable” battery backup, making it easy to move around the hospital without requiring wall gas or power outlets. With its plethora of Servo legacy functions and the gentle and sensitive non-invasive ventilation (NIV), Servo-air was thereby ideally suited for intensive and intermediary care as well as intra-hospital transportation. Servo-air proudly carries the Servo Ventilator heritage further in terms of quality, reliability, performance, ease of use and low cost of ownership.
2018 - High-Frequency Oscillation (HFO)
High-frequency oscillatory ventilation (HFOV) has become an established rescue mode for neonates with refractory respiratory failure or severe respiratory distress syndrome (RDS). Some key requirements for its integration into the Servo-n were to make it powerful through active exhalation and at the same time offer the patient reduced work of breathing [18]. The patented technology implemented is based on inertia and relies on rapid flow control and synchronization of the inspiratory and expiratory valves, managed by the legendary Servo Control System. This offers both pressure controlled and volume-targeted HFOV modes. The patient-centric solution is also supported by optional monitoring of the babies neural respiratory drive (Edi), which means that respiratory monitoring during this rescue mode is no longer guesswork.

2019 - Automatic Stepwise Recruitment Maneuver
After a number of promising clinical studies [19][20][21] that utilized Servo-i with the Open Lung Tool for stepwise lung recruitment maneuvers according to the Open Lung approach, the old dream to develop an automatic workflow finally came true. Key benefits with a standardized approach was to reduce the huge variation in clinical practice that user interviews revealed. The possibility to integrate diagnostic features which could suggest if the patient was a “recruiter” or a “non-recruiter”, is something that may have a profound effect on the ventilation strategy. Auto SRM guides the user smoothly through recruitment, decremental PEEP titration, re-recruitment and post-recruitment personalization of PEEP and Driving pressure, based on optimal Cdyn. Increased focus can be placed on finding the most adequate balance between the patient's lung mechanics, gas exchange and hemodynamics.
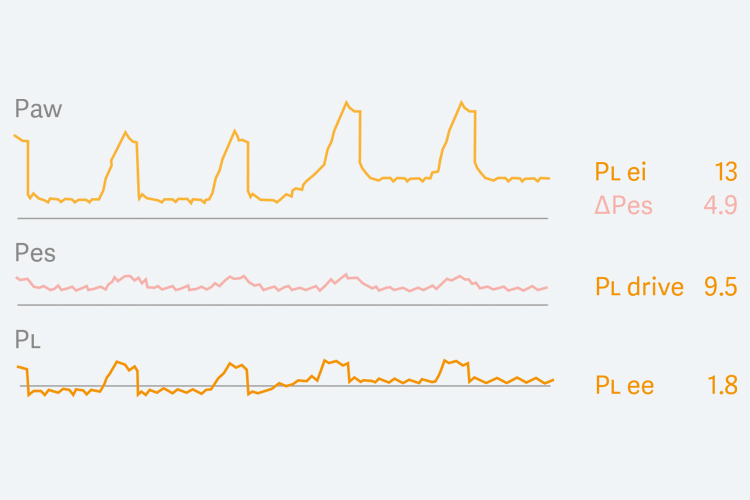
2019 - Esophageal and Transpulmonary pressure (Pes & PL)
Esophageal manometry had in the 2010s experienced something of a scientific renaissance, but was found to be difficult to implement in routine clinical use, outside the research setting. To make this technology more accessible and easy to understand and improve accuracy, a diagnostic view was developed for the Servo-u that presented esophageal (Pes) and transpulmonary (PL) pressure waveforms, with key parameters for assessment of controlled and spontaneous ventilation. In addition, an automatic occlusion maneuver was invented to validate balloon positioning and filling. This new tool for personalized lung protection has been used extensively during the Covid-19 pandemic, where it has been reported that it was now ready to be implemented in routine clinical practice.

Personalized ventilation
Every patient comes with special challenges. Whether it’s a 300-gram newborn or an adult, someone suffering from acute respiratory failure or chronic pulmonary disease, their needs and complexities will differ. That is why we are committed to innovating personalized ventilation solutions that help protect the lungs and diaphragm, speed up weaning and support better outcomes.
Over 50 years of pioneering personalized ventilation
The Servo ventilator isn’t just an engineering marvel. It’s a philosophy. A mindset, intrinsic in our DNA. It’s this conviction that has driven our pursuit in discovering new techniques in the treatment of critically ill patients. Where we are constantly evolving and reinventing our therapies and innovative solutions. The aim is to help wean the patient off the ventilator as quickly and safely as possible. Ultimately, resulting in better patient outcomes, while simultaneously using less medical resources. It’s an ambition that has remained with us from the very start, and it’s a way of thinking predominant in everything we do today. Innovation, reliability, enduring quality - doing more with less. Qualities we build into every one of our Servo ventilators produced today. It’s these same qualities that will define tomorrow’s Servo ventilators, in today’s unpredictable world. It’s how we’ve written our history. And it’s how we’ll shape our future.
